The following video shows how a knee replacement (also known as a total knee arthroplasty, TKR, or TKA) surgery is performed.
Making the choice to proceed with surgical management for knee arthritis can be very daunting. This decision should be taken very seriously by both the patient and the surgeon. Typically, patients will have failed multiple conservative measures conservative measures and will need to be a good medical candidate medical candidate for surgery.
My Knee Guide is committed to providing the most comprehensive resources for patients who are considering or undergoing a FULL (or total) knee replacement; however, it is important to understand that other options that may be discussed with your surgeon. These include:
- Arthroscopy Arthroscopy - It is generally not recommended to "scope" a knee to "clean up" arthritis. However, there can be benefit in limited cases such as for removal of a symptomatic loose body, or trimming a torn meniscus. Arthroscopy may be used to assist with cartilage restoration procedures described below. Arthroscopy for severe arthritis is rarely indicated.
- Partial knee replacement Partial knee replacement - also called a “uni”, “medial”, or “lateral” compartment replacement. This procedure will reconstruct either the inside or the outside portion of the knee. Additionally, another option is to replace only the knee cap region (patella-femoral) if there is isolated arthritis in this part of the joint.
- Re-alignment procedure such as an osteotomyosteotomy.
- Cartilage restoration procedure Cartilage restoration procedure such as an abrasion arthroplasty or osteochondral transplant.
My Knee Guide recommends for each patient to make the decision for the type of procedure, collaboratively with the guidance of their orthopaedic surgeon. There are many clinical factors that a surgeon will evaluate before recommending the particular procedure, such as x-raysx-rays (perhaps even an MRI), pain levels, ligament stability, deformity, surgical history, patient’s age and activity level. You can also read a surgeon's perspective relating to 'When Should I Have My Knee Replaced''When Should I Have My Knee Replaced'.
There are more than 700,000 total knee replacements performed annually in the United States alone and it is one of the most successful procedures performed. Approximately 90% of patients obtain excellent outcomes from surgery. Total knee replacement has been shown effective in relieving pain, correcting knee deformity, improving function, preserving independent lifestyle, and contributing to psychological well being. A recent analysis of the best studies evaluating post-operative health-related quality of life indicators has demonstrated that the substantial benefit to mental as well as physical health after total knee replacement are maintained over time.66
To find out more about how knee deformity can be corrected with knee replacement surgery read 'Will my knee be straightened with surgery?''Will my knee be straightened with surgery?' on BoneSmart.org.

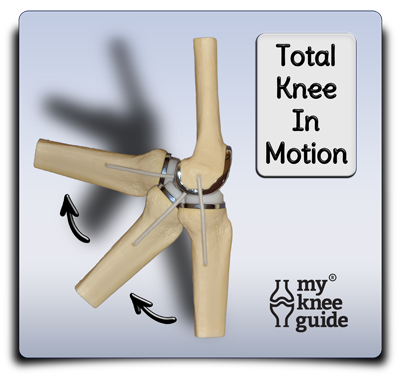
The technology behind modern total knee replacement continues to evolve and improve. Current studies show that replacements that were performed 10 years ago have a survivorship of 90%-98%, 15 years ago have a survivorship of 80%-95% and those performed 20 years ago have 75% survivorship rate. Since modern components keep improving, it is expected that these survivorship rates may improve as well.
Over the last twenty years there has been a huge amount of research and development dedicated to improve knee replacement surgery. This includes research into the metal and plastic components that are used to create the knee prosthesisknee prosthesis, along with the instrumentation used to implant them. Additionally, there have been changes in the surgical techniques used for exposure of the soft tissues, bone, cartilage and ligaments during surgery.
These changes in components, instrumentation and surgical techniques have become the focus of marketing campaigns surround knee replacement surgery. It is important to have good perspective and understanding when reading about these changes. Ultimately, the experience of your surgeon and your particular medical condition will factor more heavily in obtaining an excellent outcome, when compared to the all of these changes in techniques and equipment. Your orthopaedic surgeonorthopaedic surgeon will be an excellent source to help determine if any of these apply to your clinical situation.
Minimally Invasive Surgery
When the surgical technique was originally described for the knee replacement, there was an emphasis on obtaining maximal exposure to be able to perform the surgery as well as possible. As time progressed and excellent outcomes from surgery were becoming more routine, surgeons decided to reduce the size of the incision and modify how the soft tissues were handled. This was done in an effort to disrupt fewer muscles and tendonsmuscles and tendons, with the assumption that this would decrease pain and swelling, and improve outcomes.
Around the time of the late 1990s, surgeons developed minimally invasive surgical techniques (MIS) as a result of this trend to reduce incisionincision size. However, in an attempt to create very small incisions, surgeons were sometimes not able to obtain adequate exposure to the joint and increased the chance that the component was placed in the improper position. This has led most surgeons to become more selective in whom they would use a very small incision. This may be based on the patient's body type, amount of knee deformity and mobility of the soft tissues.
Initially the studies of the early post-operative period using MIS techniques were very promising. They found decreased pain and earlier discharge from the hospital. However, over time it was discovered that these factors were also dependent on concurrent changes to post-operative therapypost-operative therapy protocols and the addition of multi-modal pain managementmulti-modal pain management. Studies that focused on long term outcomes (rather than early post-operative recoveryrecovery) ultimately did not show significant differences in the outcomes of patients compared to traditional incisions.
Based on these findings, most surgeons have adopted some parts of minimally invasive techniques into their procedure and are more cognizant of careful soft tissue handling. However, there is now less emphasis on creating the smallest possible incision.
Computer Navigation
Around the time that minimally invasive techniques were being pioneered, surgeons were looking for ways to improve the accuracy of component positioning. Proper positioning of the components is critical to obtaining excellent function of the knee replacement and to reduce the chance of failure of the components over time. The position of the components will determine the alignment of the leg after surgery and is responsible for straightening a crooked knee due to arthritiscrooked knee due to arthritis.
Surgeons developed a technique that would use various markers on the leg which would allow a computer to help guide bone cuts and soft tissue balancing to achieve a neutral (well aligned) position for the knee replacement. This could be used instead of or in conjunction with tradition jigs and guides used during surgery.
The results of the studies using computer navigation were rather mixed as to the effectiveness of this technique. Some studies showed improvements in alignment (although typically only small improvement) and others did not show any significant differences. When surgeons use this technique there is an increased operative time (to apply and use the computer navigation) along with increased associated costs. For these reasons, the use of computer navigation has not become routinely used by most surgeons.
Patient Specific Instrumentation
More recently, orthopaedic implant companies have increased efforts to individualize the surgical procedure to the patient's specific anatomy. As described earlier, orthopaedic surgeons use intra-operative jigs and guides to create the cuts in the bone to align the knee correctly. Currently, there is a new method for creating these bone cuts with the use of a patient specific guide.
This guide is fabricated by the joint replacement company based on a pre-operative analysis of the patient's anatomy using a CT scan or MRI scan. This guide is then delivered to the surgical suite where the surgeon will use it, rather than using a traditional guide, to make the bone cuts.
There are some advantages to using this technology. They include the potential for slightly shorter operative time and the need for less instrumentation in the operating room. Also these types of guides may be particularly useful in patients who have had previous surgery or injury to the thigh bone (femurfemur), where the use of the traditional guide would not be possible.
However there is an added cost to fabricate a custom guide for each patient. Also, the systems that use a CT scan to fabricate the guide, exposes the patient to extra (potentially harmful) radiation. The recent studies have been mixed on the effectiveness of these guides and have not shown significant improvement of knee alignment or patient outcomes.11,55,66
Gender Specific Implants
Is there any benefit or need to have a gender specific knee? Theoretically, there are some differences in the anatomy of the knee based on gender. These include the size of the bone, rotational differences and differences in the alignment of the knee cap.
Zimmer® has designed a implant that is marketed to be more specific to these subtle anatomic differences between a female and a male knee. They have adjusted their knee replacement componentknee replacement component by modifying the thickness of the metal, and changing its contoured shape.
Question one: "Is there a difference in the outcomes of men and women using traditional (non-gender specific components)?" The answer is that studies have not shown consistent differences between the sexes as related to failure of the prosthesis, range of motion or overall outcome.22
Question two: "Do women with gender specific knee replacements have better outcomes?" One specific study looking for this answer found no evidence of any advantage in range of motion, "feel" of the knee, pain or satisfaction with the use of a gender-specific designed prosthesis.33
Robotic Surgery
Robotic surgery in orthopaedics was originally pioneered in the early 1990's. One of the main theoretical benefits of this technology is the ability to create more accurate bone cuts and reproduce the correct alignment of the leg. There are have been some studies that show promising results that robot assistance may reduce the number of patients that have a mal-positioned component.44 This technology has been used successfully for partial (uni) replacements for many years. More recently, robots are being used in the operating room to assist the surgeon during a complete or full knee replacement.
It is too early to draw any accurate conclusions on whether these systems will improve the outcomes of these patients. There are some potential drawbacks to the use of robotic assisted surgery. Some systems still rely on the use of pre-operative advanced imaging (CT or MRI scans) and can increase the risk of radiation to the patients. Each of these systems add significant costs to the surgery (or to the hospital for purchase of the equipment) compared to the current methods. Additionally, there is a steep learning curve for the surgeons when they start using the system. Another important consideration is that there is added operative time with using a robot as well.